Hypersensitivity in fibromyalgia
Hypersensitivity in fibromyalgia isn’t the same things as being “too sensitive” in the way people usually mean when they throw that phrase around. It’s not that we’re emotionally fragile, it’s that our physiological response is bigger than most people’s, and over the years researchers have learned more about how the brains of people with fibromyalgia respond or rather, over-respond to changes going on around us.
We’ve known for a long time that fibromyalgia involves abnormal hypersensitivity. The most obvious thing we’re hypersensitive to is pain, but it doesn’t stop there heat, cold, noise, lights, smells, crowds, motion, chaos also cause discomfort. This hyper-responsiveness, when it has to do with pain, is called hyperalgesia.
Hyperalgesia is a conditions that include this feature have recently been classified under the umbrella of central sensitivity syndromes since the symptom stems from dysfunction in the central nervous system. Ongoing research gives us insight into why and how we have this exaggerated response.
Researchers from the University of Michigan and South Korea’s Pohang University of Science and Technology say they’ve found evidence of something called “explosive synchronization” in the brains of people with fibromyalgia.
Explosive synchronization (ES)
A new study finds that patients with fibromyalgia have brain networks primed for rapid, global responses to minor changes. This abnormal hypersensitivity, called explosive synchronization (ES), can be seen in other network phenomena across nature. Researchers from the University of Michigan and Pohang University of Science and Technology in South Korea report evidence of ES in the brains of people with fibromyalgia, a condition characterized by widespread, chronic pain.
Let put this on our cars and spread Fibromyalgia Awareness
– Click Here to get Yours Fibromyalgia Disability Sticker for you Car
The paper, published in Scientific Reports, details only the second study of ES in human brain data. “For the first time, this research shows that the hypersensitivity experienced by chronic pain patients may result from hypersensitive brain networks,” says co-senior author Richard Harris, Ph.D., associate professor of anesthesiology at Michigan Medicine with the Chronic Pain and Fatigue Research Center. “The subjects had conditions similar to other networks that undergo explosive synchronization.”
Electrically unstable’ findings
The researchers recorded electrical activity in the brains of 10 female participants with fibromyalgia. Baseline EEG results showed hypersensitive and unstable brain networks, Harris says. Importantly, there was a strong correlation between the degree of ES conditions and the self-reported intensity of chronic pain reported by the patients at the time of EEG testing.
Lee’s research team and collaborators in South Korea then used computer models of brain activity to compare stimulus responses of fibromyalgia patients to the normal condition. As expected, the fibromyalgia model was more sensitive to electrical stimulation than the model without ES characteristics, Harris says. “We again see the chronic pain brain is electrically unstable and sensitive,” Harris says. He says this type of modeling could help guide future treatments for fibromyalgia.
Since ES can be modeled essentially outside of the brain or in a computer, researchers can exhaustively test for influential regions that transform a hypersensitive network into a more stable one. These regions could then be targeted in living humans using noninvasive brain modulation therapies.
A small stimulus can lead to a dramatic synchronized reaction
In ES, a small stimulus can lead to a dramatic synchronized reaction in the network, as can happen with a power grid failure (that rapidly turns things off) or a seizure (that rapidly turns things on). This phenomenon was, until recently, studied in physics rather than medicine.
Researchers say it’s a promising avenue to explore in the continued quest to determine how a person develops fibromyalgia. As opposed to the normal process of gradually linking up different centers in the brain after a stimulus, chronic pain patients have conditions that predispose them to linking up in an abrupt, explosive manner,” says first author UnCheol Lee, Ph.D., a physicist and assistant professor of anesthesiology at Michigan Medicine. These conditions are similar to other networks that undergo ES, including power grids, Lee says.
The Underlying Mechanism
When doctors set out to understand a condition, the “underlying mechanism” of that condition is an important thing to figure out. It’s the answer to why the body is behaving as it is. Without understanding the underlying mechanism, it’s like trying to repair a broken car without knowing which part is broken.
If ES is the underlying mechanism behind the hypersensitivity of fibromyalgia, then treating ES would be far more effective than using drugs to dull the pain—it could, finally, be the thing that goes beyond the symptoms and corrects the physiology that’s gone awry.
Of course, one small study is never conclusive. It’ll take years of work to know for sure whether this theory is accurate, and then more time to figure out the best ways to treat it. However, if these researchers are right, this could be a crucial first step toward better outcomes for people with fibromyalgia.
The insights may also stretch beyond fibromyalgia
The study not only points the way to the potential alleviation of hypersensitivity in brain networks, but it also shows the power of computer models of the brain, which could have implications for personalized medicine, as it could allow physicians to see how a given therapy might work before trying it with a particular patient.
The insights may also stretch beyond fibromyalgia, according to the study’s co-senior author Richard Harris, PhD, a University of Michigan associate professor of anesthesiology, and part of the university’s Chronic Pain and Fatigue Research Center.
“Our group and others suggest that the hypersensitive brain seen in fibromyalgia patients is likely to present in many other pain conditions,” he said. “For example, increased functional neural connectivity, an outcome that may be related to explosive synchronization, between the sensory cortex and other brain networks transcends multiple pain diagnoses.”
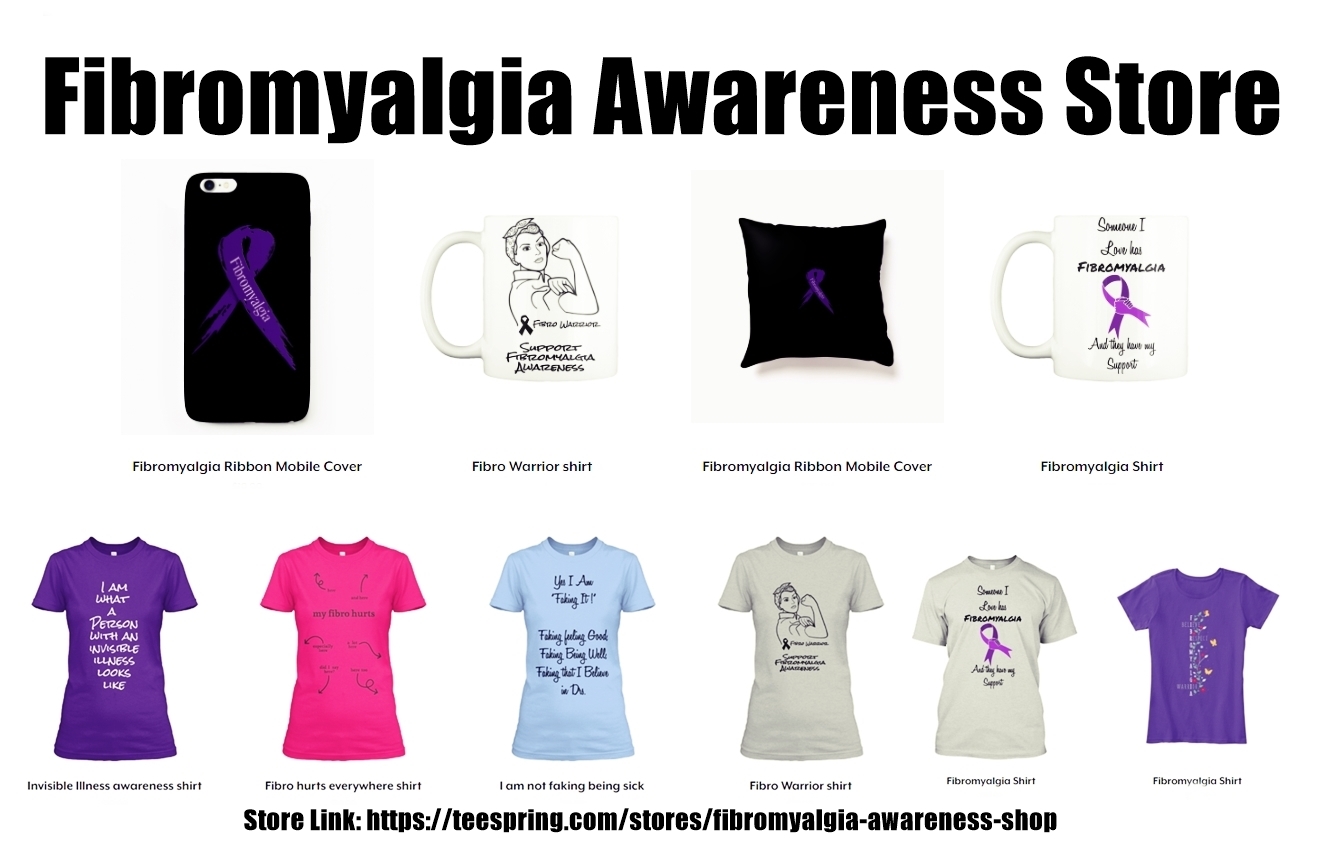
Fibromyalgia Awareness Store: With so many people across the world affected by the pain, fatigue and brain fog of fibro, it is critical we raise awareness of the condition.Along with speaking, lets spread out fibromyalgia awareness with some others means, let the things speak out it self. Like you can have customized T-Shirts, Mugs, Stickers, Pants, Mobile Covers, Socks, Wall Tapestry. Click Here to visit the Store
Click Here to Go to Store
Reference : The study, “Functional Brain Network Mechanism of Hypersensitivity in Chronic Pain,” was published in the journal Scientific Reports.